Doctors at Pittsburgh medical center clash with hospital administrators over coronavirus policy
A Pittsburgh-based hospital system faces growing dissension from hundreds of its doctors over its controversial decision to continue routine clinic visits and certain elective surgeries in the face of COVID-19.
More than 300 medical residents, fellows and attending physicians at the University of Pittsburgh Medical Center (UPMC) signed an open letter to administrators of the $21 billion nonprofit hospital system and insurer, which owns 40 hospitals and hundreds of clinical locations and outpatient facilities — principally in Pennsylvania, but with outposts in Ireland, Italy and China.
The doctors urged administrators to reverse course and delay “truly non-urgent outpatient appointments and elective surgeries” in light of the continued uncertainty about the prevalence of the coronavirus in their community, the risks to hospital staff and other patients of contracting the virus from undiagnosed carriers, and the need to conserve personal protective equipment and ventilators that are already in short supply.
“While we understand the financial implications inherent in keeping patients at home,” the doctors wrote, “the benefits clearly outweigh these risks in the context of a global pandemic.”
The UPMC doctors’ letter was delivered to administrators on Wednesday, March 18, and continued to gain signatories through the weekend. As of Monday, more than 300 doctors had signed the letter.
While the doctors stressed the immediate issues of arresting the spread of COVID-19 and preserving limited resources, UPMC’s administrators appear more focused on putting the hospital on a long-term footing.

Yahoo News also obtained an internal policy document issued by UPMC administrators that makes the case that the hospital system needs to learn to live with COVID-19 for months to come.
The administrators wrote that they expect COVID-19 cases to persist “for the foreseeable future,” and therefore “balancing the ongoing clinical needs of our patients with avoidance of unnecessary exposure requires a nuanced approach — not an across-the-board cancelling of clinics and procedures.”
Dr. Amesh Adalja, a specialist in emergency medicine and a senior scholar at the Johns Hopkins University Center for Health Security, agreed that hospitals need to “take a nuanced approach” to managing elective procedures, informed by the spread of the outbreak in the surrounding area and the resources the hospital has available.
An elective procedure is one that can be scheduled in advance, though that doesn’t necessarily mean it’s optional. “People use the word ‘elective,’ and the public thinks that’s cosmetic,” Adalja said, pointing out that elective procedures range from cosmetic procedures to operations for life-threatening conditions, like biopsies to detect cancer. As they cope with the COVID-19 outbreak, “hospitals need to look at the needs of the patient population they serve,” Adalja said.
No experts consulted by Yahoo News disagreed that some elective procedures are so important to a patient’s health that they ought to go forward. However, they explained that acknowledging that need does little to resolve the difficult policy questions that health care providers face.
“We’re facing a really unprecedented situation here,” said Dr. Ashwin Vasan, a primary care physician and public health professor at Columbia University. “Hospitals and health systems have never been faced with the impending level of potentially serious and critical cases that could result from the pandemic. Hospitals and health systems aren’t currently really set up for this level of acuity all at the same time. … So anyone who’s saying, ‘Hey, business as usual has to keep going on’ is not really appreciating the dimensions and the scale and the severity of this pandemic.”
Writing to medical staff, UPMC administrators said that “elective procedures should only be delayed when, in your expert opinion, it is clinically safe to do so. It is likely COVID-19 will be in our community for months, and safely rescheduling non-urgent visits/procedures may require at least 8-10 weeks. Put another way, if it is not safe to delay a visit or procedure that long, the patient should receive care sooner.”

In a separate email, Gregory Bump, UPMC’s chair of graduate medical education, wrote to residents and fellows that “elective surgeries should be continued to maintain the health of patients with time sensitive surgeries.”
Bump said such elective surgeries might include surgery to remove a cancerous growth. “I am confident you can envision other ‘elective’ procedures that are not emergent but clearly time-sensitive,” he wrote.
Vasan agreed that something like a cancer surgery should go forward, but he said, “What you have to remember is that there are a number of less-urgent and elective procedures that people do at hospitals all the time, and you have to remember that these are massive, revenue-generating things.”
The UPMC policy document urges medical staff to accept the danger to themselves from the COVID-19 outbreak, unless their own age or other medical conditions compel them to stop practicing.
“We have a responsibility to the public to provide care — even at risk of personal harm,” the UPMC administrators wrote, adding, “If you feel your personal health requires you to stop practicing while COVID-19 is uncontrolled for reasons of co-morbidity or age we are supportive.” The administrators did not address whether health care workers’ concerns about inadequate testing or equipment shortages would receive the same support.
UPMC has persisted in its policy despite an order from Pennsylvania’s governor that prohibits “elective procedures” in hospitals and other medical facilities within the state, insisting it interpreted the governor’s order as not applying to “necessary” elective procedures.
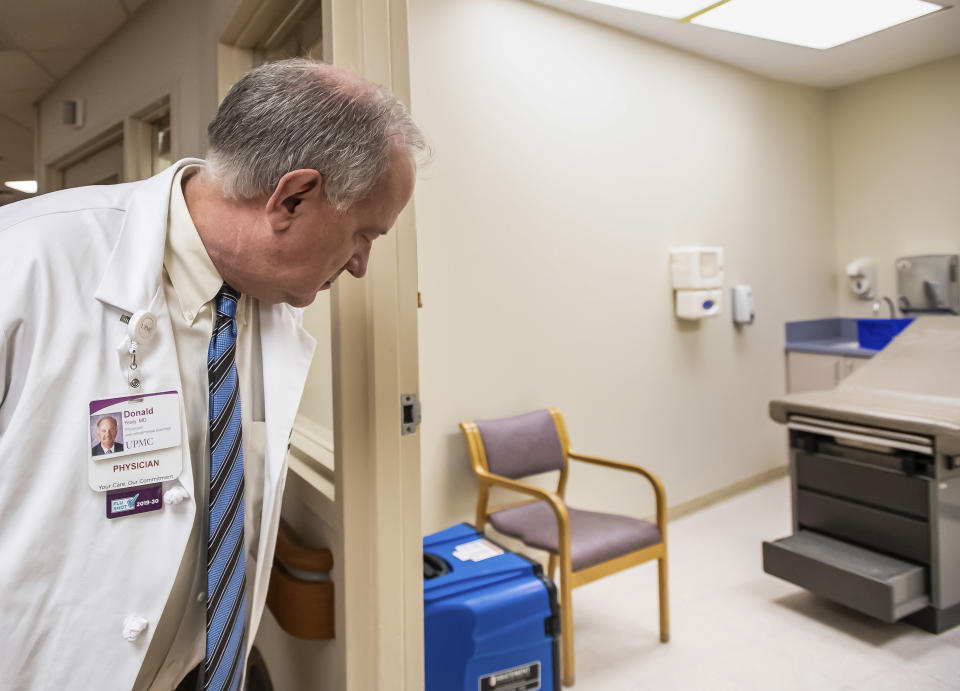
At a press conference on Friday, Dr. Donald Yealy, UPMC’s chair of emergency medicine, and other UPMC administrators defended their decision to continue elective procedures. “Elective commonly means scheduled cases, but scheduled does not mean unnecessary,” Yealy said. “The governor and CMS did not request that necessary care be canceled.”
The Pennsylvania governor’s office and the Pennsylvania Department of Health did not respond to messages seeking comment over the weekend, but the Allegheny Health Department reiterated the governor’s directive that UPMC “wind down elective procedures as soon as possible” in an interview with the Pittsburgh Business Times.
To back up their decision, the UPMC administrators cited a recent survey that showed only five confirmed COVID-19 cases among 950 subjects in the Pittsburgh area. They also reported that “across the UPMC system, 28 symptomatic patients have tested positive, with four of those people currently hospitalized.”
“Many scheduled care opportunities, often called elective, whether that be cancer care, valve replacement in the heart, or hernia repair, address important health care needs that can’t always be safely delayed,” Yealy said. “We are continually monitoring COVID cases, both test-proven and suspected, in our facilities and in the region. Fortunately, right now, both remain low.”
The UPMC doctors who signed the letter disagreed, arguing that broader cancellations of clinic visits and elective surgeries make sense in light of the crisis.
The doctors wrote that COVID-19 testing is simply not robust enough to establish whether it is spreading in the Pittsburgh area, because of the lack of testing kits. The doctors argued that important cohorts of people are not being tested, including patients who are symptomatic and have recently traveled domestically, patients who have traveled internationally to a known hot zone but are not symptomatic and health care workers themselves.
The doctors also wrote that it’s “imperative that we limit the number of people moving through our healthcare system to preserve critical resources,” and that certain operating room necessities, such as surgical gowns and towels, are “now in limited supply.”
UPMC did not respond to a detailed list of questions from Yahoo News but offered a general statement: “We appreciate, understand and embrace the concerns and the potential solutions offered by all at UPMC,” wrote Courtney Caprara, a spokesperson for the hospital system.
A pulmonologist practicing outside the UPMC system, who asked not to be named due to their employer’s policy, agreed with the overarching argument of the open letter. “This is a critical time for intervening to prevent a surge,” the pulmonologist said. “It’s not just about the care, it’s about protecting your institution by having less people around and therefore less chance that someone will bring infection in — social distancing, but for health care workers. Basically, you want to keep your decks clear for the surge of sick people, but also want to keep your people healthy right now.”
Both sides in the debate appear to face the same problem: a lack of good data on the implications of any specific policy.
“This is a very tough call,” said John Ioannidis, a professor of epidemiology and disease prevention at Stanford University. “And the problem is that if we don’t have data — which we don’t — on the exact prevalence of the infection at the moment, any decision will be mostly guesswork. So it’s a bit in the blind that we need to decide.”
_____
Read more from Yahoo News:


